Oophorectomy: Everything you need to know
By Jon Johnson
Reviewed by Debra Rose Wilson, PhD, MSN, RN, IBCLC, AHN-BC, CHT
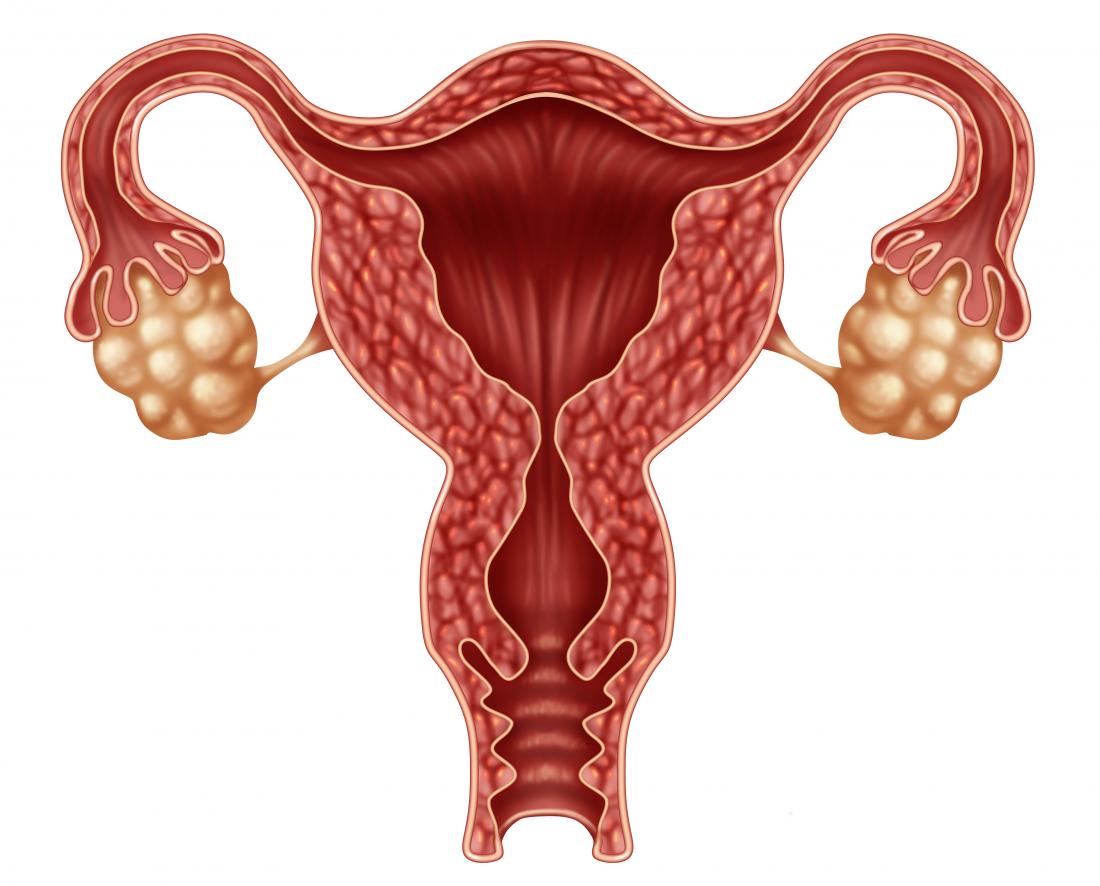
An oophorectomy is a surgical procedure to remove one or both of a woman's ovaries. The surgery is usually performed to prevent or treat certain conditions, such as ovarian cancer or endometriosis.
An oophorectomy comes with its own risks and complications, so a person should always discuss their options with a doctor prior to surgery.
The surgery only lasts a few hours, but recovery times can vary. Self-care is an important part of recovery, and it is crucial to discuss recovery with a doctor beforehand to avoid unwanted complications.
What is an oophorectomy?
The term oophorectomy is used to describe the surgical removal of one or both of the ovaries. It is also called ovariectomy.
The surgery may just remove the ovaries, or it may be a part of a hysterectomy, which is the removal of the uterus and possibly some surrounding structures.
There are different reasons for an oophorectomy, including:
- treating abnormal tissue growth from endometriosis
- lowering the risk of ectopic pregnancy
- treating pelvic inflammatory disease (PID)
- removing ovarian cysts, abscesses, or cancerous cells in the ovaries
- removing the source of estrogen, which may stimulate some cancer, such as breast cancer
Women who carry the BRCA1 or BRCA2 genes may be more likely to experience certain types of cancer and may choose to have an oophorectomy, as a preventive measure.
Types of oophorectomy
Oophorectomy is a broad term for a medical procedure that removes one or both ovaries, but there are different types of oophorectomies that can be done.
- Unilateral oophorectomy: Removal of one ovary, usually done when a woman still wants to become pregnant.
- Bilateral oophorectomy: Removal of both ovaries, done to prevent disorders or spread of cancer cells.
- Salpingo-oophorectomy: Removal of the fallopian tube along with the ovary, often to treat cancers or other disorders.
- Prophylactic oophorectomy: Also called a preventative oophorectomy, this procedure is done to reduce the risk of future diseases.
What to expect
A person should always discuss what to expect during and after the surgery with their doctor.
Several tests may be used before scheduling the operation, including:
- physical exams
- blood tests
- urine tests
- computed tomography (CT) scan
- ultrasound
An oophorectomy is performed using either open abdominal surgery or laparoscopic surgery. Both operations should take no more than a few hours to complete but may require staying one or several nights in the hospital.
Open abdominal surgery
In an open abdominal surgery, a surgeon will make an incision in the abdomen and then carefully separate the abdominal muscles.
Blood vessels will be temporarily tied off to prevent bleeding. The surgeon will remove the ovary or ovaries and then seal up the incision.
Laparoscopic surgery
During laparoscopic surgery, a thin, cord-like instrument is inserted into a small cut near the navel. A tiny camera allows the surgeon to see and remove the ovary or ovaries.
The process may leave less noticeable scars and have a shorter recovery time than open abdominal surgery.
After the surgery
It is helpful for someone else to drive the woman home and care for her in the first few days after her surgery.
Most surgeries will require at least 2–3 weeks away from work. Regular check-ups allow doctors to monitor and alter the recovery process, as needed.
How long does recovery take?
Recovering from an oophorectomy will vary based on a few different factors, including the type of surgery. Laparoscopic surgery may require only 1 day in the hospital, but open abdominal surgery will typically need 2 or more days in the hospital.
Recovery recommendations will vary, depending on the individual, but some general recovery tips include:
- resting before surgery and during recovery
- taking relaxed, deep breaths
- avoiding heavy lifting or exercise
- refraining from sexual intercourse
- avoiding using tampons during recovery
- making dietary changes and taking medications for constipation as needed
- avoiding infection risks, such as taking baths and wearing tight or synthetic clothing
Doctors will also instruct their patients on how to take care of their incision site, including regular cleaning, keeping the area dry, and monitoring it for signs of infection.
Risks and complications
Although an oophorectomy is often performed to help treat or prevent diseases, it may put women at risk of other issues.
Serious complications are rare, but people who smoke, are obese, or have diabetes may be more at risk for surgical complications.
Women who have had pelvic surgery or serious infections in the past may also be more vulnerable to complications.
Women who have both ovaries removed will no longer be able to become pregnant. A woman who wishes to become pregnant or is considering pregnancy in the future should discuss alternative options to oophorectomy with a doctor.
Signs of complications
It is vital to report any signs of a complication to a doctor, as soon as possible. These signs and symptoms include:
- fever
- abnormal amount of blood or discharge
- redness and swelling near the incision
- skin near the incision feeling very warm
- nausea and vomiting for more than a few days
- difficulty urinating
- chronic abdominal pain
- shortness of breath or chest pain
- mood swings
- depression
The surgery itself also involves some risks, including:
- excessive bleeding or blood clots
- infection
- scar tissue
- nerve damage
- tumor rupture
- injury to the urinary tract or other organs
- hernia due to weakened abdominal muscles
In rare cases, people may experience respiratory or cardiac problems after anesthesia.
Hormonal changes
Women who have both of their ovaries removed before they have reached menopause usually take hormones to reduce the risk of menopause symptoms or other disorders. Hormone therapy, comes with side effects, however, including mood swings, nausea, and headaches.
A woman may choose to let the body go through menopause without taking replacement hormones. It is best to discuss any potential hormonal changes with a doctor before an oophorectomy. Some women will be treated with hormones, but not all are good candidates.
Osteoporosis
A bilateral oophorectomy may also increase the risk of a woman developing osteoporosis, which causes weak and brittle bones. This is because the body will no longer produce much estrogen.
Osteoporosis can increase the risk of breaking bones, particularly from falls or other injuries.
Life expectancy
Women who keep their ovaries until at least the age of 50 may live longer than women who have a bilateral oophorectomy before then.
One study noted that while a bilateral oophorectomy does reduce the risk of death from ovarian cancer and breast cancer in some cases, it may increase the risks of death from all other causes.
However, surgery may still be the best option for women who are BRCA1 or BRCA2 carriers.
A review in the Journal of Clinical Oncology noted that women with these genes who have their ovaries removed have an 80 percent reduction in the risk of death from specific cancers and a 77 percent reduction in risk of death from all causes.
It is essential for a person to discuss their personal history and all their options with a doctor before choosing an oophorectomy.
Outlook
An oophorectomy can be a lifesaving procedure in many cases. However, women with an otherwise healthy uterus and ovaries should thoroughly discuss their options with a doctor, as the surgery comes with some risks.
Women should give themselves plenty of time to recover from surgery, as the recovery time can vary. A woman may want to consider having help at home for the first few days to assist her getting up and preparing meals.
Women who have had one ovary removed but still have their uterus may notice very little change, as their hormones and menstruation will stay relatively the same. Women who have had both ovaries removed will notice the biggest change.
Doctors can help people to explore recovery options and give them more information about what symptoms to expect after an oophorectomy.
SOURCE: MEDICAL NEWS TODAY
Comments
Post a Comment